It's your health. Be breast informed.
Learn about the risks of dense breasts, breast screening policies in your province, the latest evidence, and how to advocate for the screening you need.
Make the best decisions for your health. We are here to help.
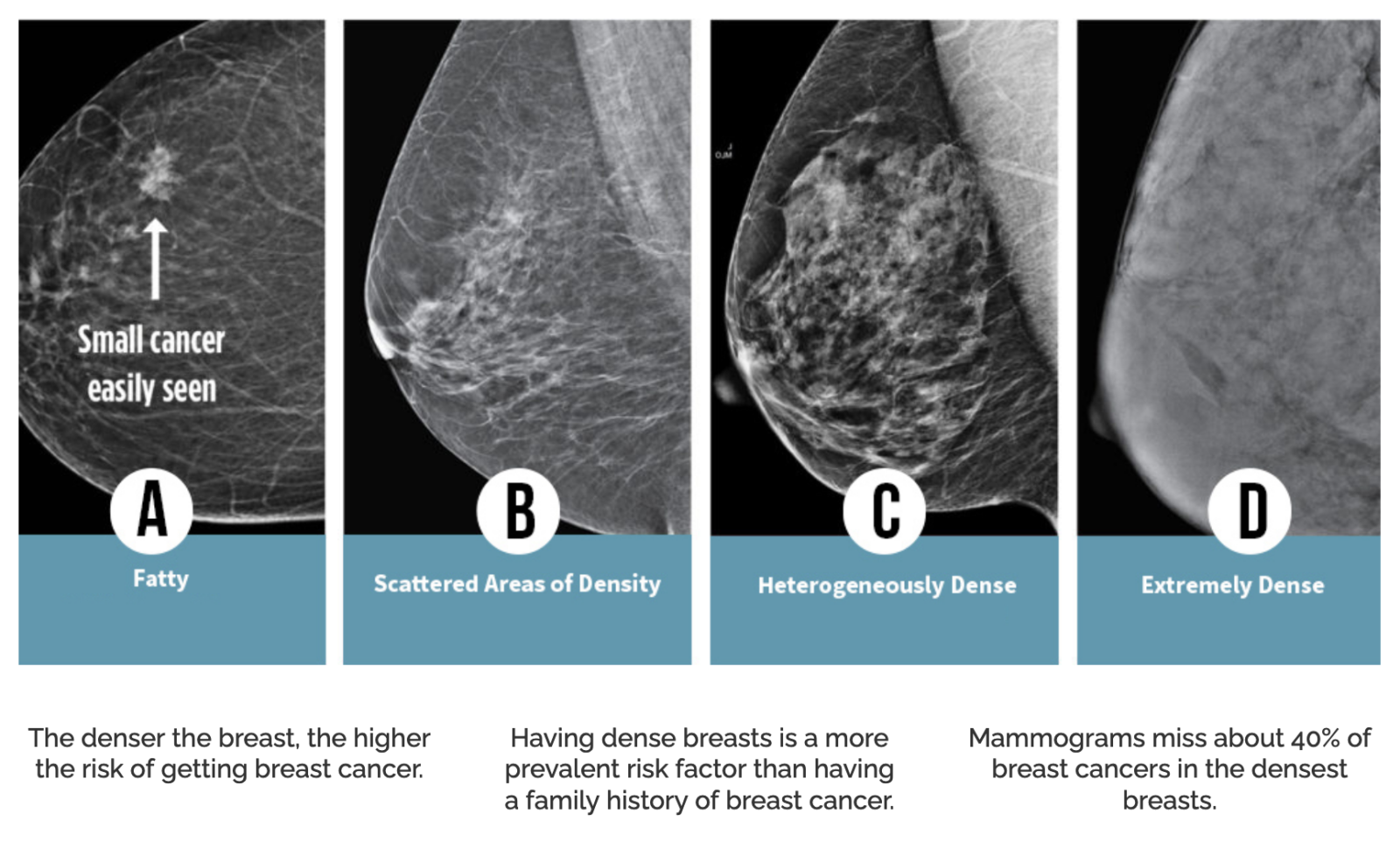
Dense breasts increase your risk for breast cancer and dense breasts make it difficult for breast cancer to be seen on a mammogram. You can take steps to minimize your risk. Know and understand your breast density.
Four Categories of Breast Density

Renseignez-vous facilement sur les pratiques du programme de dépistage de votre province ou territoire, sur les dernières recherches menées par les experts du cancer du sein et sur la manière de plaider en faveur du dépistage dont vous avez besoin.
Read the powerful stories of those with lived experience with breast cancer and what they would like those WITHOUT breast cancer to know.


Learn how you can advocate for your own heath and breast screening needs. One size does not fit all when it comes to screening. Understand your risk and the screening that is best for you so you can advocate for it.
In May, 2024, The Canadian Task Force on Preventive Health Care (Task Force) released its draft breast cancer screening guidelines. Dense Breasts Canada is deeply concerned about the dangerous guidelines. DBC has met with government officials, testified to federal committees, written Op-Eds, and will continue to have discussions with the government. We are getting closer to seeing change. Read about our concerns.