What Is Breast Density?
Each woman’s breast composition is unique. Every woman has fat, glands and fibrous tissue in her breasts, but the proportions of each vary from woman to woman and cannot be seen without a mammogram. There are 4 categories of breast density.
Each woman’s breast composition is unique. Every woman has fat, glands and fibrous tissue in her breasts, but the proportions vary from woman to woman.
Breasts that have more glandular and fibrous tissue are called dense breasts.
Dense breasts are common. For women aged 40-74 years, 43% have dense breasts. Breasts usually become less dense and fattier with age:
- 56% of women in their 40s have dense breasts.
- 37% of women in their 50s have dense breasts.
- 27% of women in their 60s have dense breasts.
It is normal to have dense breasts. However, women need to know if they have dense breasts so that they can understand the risks and implications and make informed screening decisions.
You need to have a mammogram to learn your breast density. Breast density is determined by the radiologist reviewing your mammogram. Automated software can also calculate the breast density, but is only used in a few provinces. Breast density is NOT determined by the size or firmness of your breasts. You cannot tell density by look or feel. Some health practitioners after a clinical exam will tell women they have dense breasts, but it is not possible to know from feel.
Dense breasts are not the same as lumpy breasts.
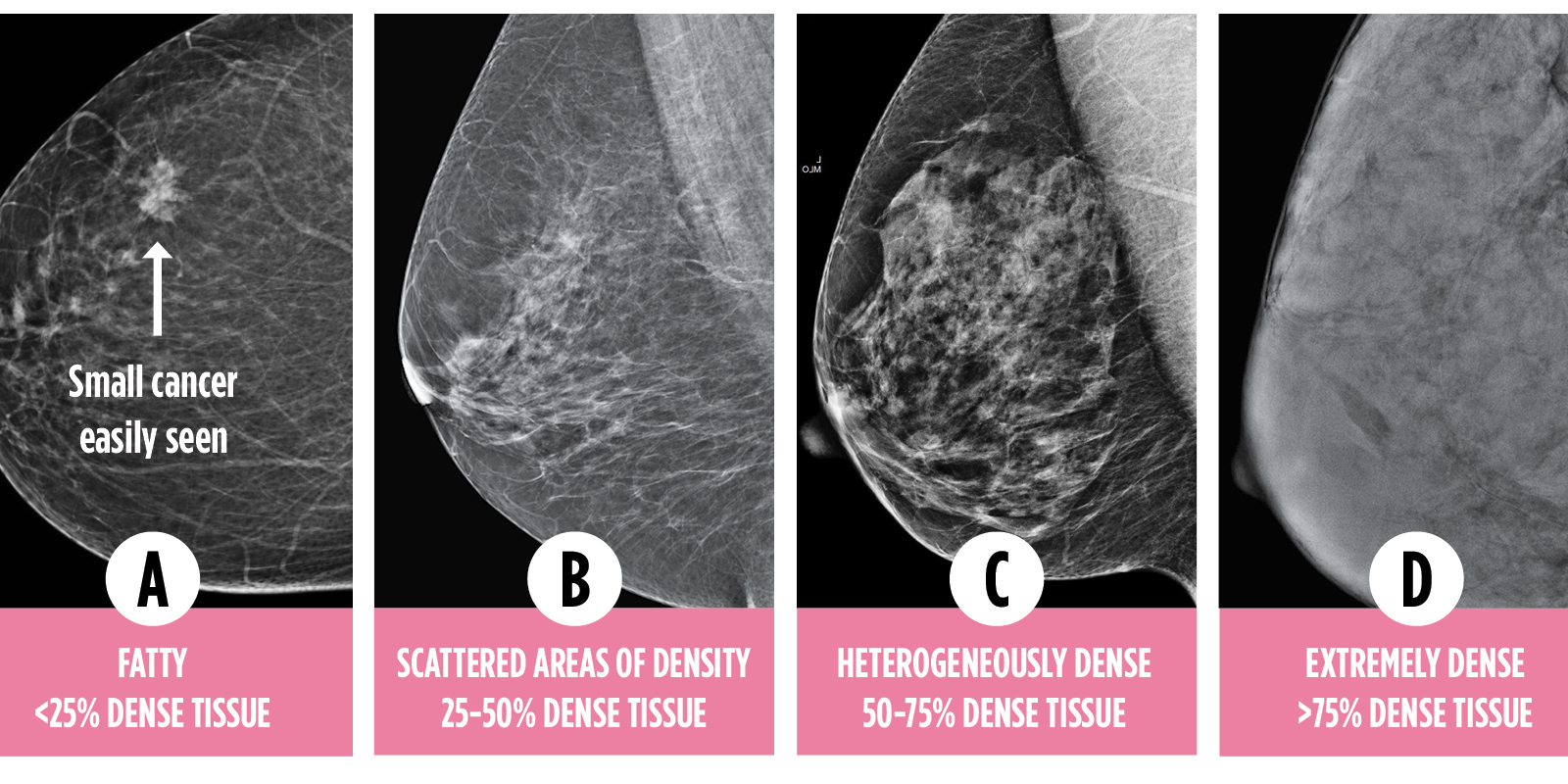 Breast density is a continuum and is described as one of four categories: A, B, C, or D. Some provinces describe the categories in words as well.
Breast density is a continuum and is described as one of four categories: A, B, C, or D. Some provinces describe the categories in words as well.
CATEGORY C and D ARE CONSIDERED DENSE BREASTS.
Dense breast tissue may obscure small tumors and make a mammogram less accurate.
Category A | Almost entirely fatty
The breasts have little fibrous and glandular tissue and are mostly fat. A mammogram would likely detect an abnormality.
Category B | Scattered areas of fibroglandular density
The breasts have scattered areas of fibrous and glandular tissue, but also quite a bit of fat.
Category C | Heterogeneously dense
The breasts have consistently distributed areas of fibrous and glandular tissue, making it hard for small masses to be detected by mammogram.
Category D | Extremely dense breasts
The breasts have a lot of fibrous and glandular tissue, making it even harder for a cancerous tumor to be detected by mammogram.
Which category are you in? You'll need a screening mammogram to find out.
The following are estimates and may vary by province depending if the province uses software to assess the density on a mammogram or if it is assessed subjectively by the radiologist.
- 10% of women have the lowest category of density known as ‘Fatty’ breasts
- 40% have ‘Scattered areas’ of density
- 40% of women fall in the category Heterogeneously Dense Breasts/Category C (considered dense breasts).
- 10% of women fall in the highest category ‘Extremely Dense/ Category D (considered dense breasts).
The higher the density, the higher the risk of breast cancer and that a tumour will be missed.
AGE: Dense breasts are more common in younger women. As women get older, their breasts usually become less dense, but not always.
- 56% of women in their 40s have dense breasts.
- 37% of women in their 50s have dense breasts.
- 27% of women in their 60s have dense breasts.
MENOPAUSE: Density usually decreases after menopause, but not always.
ETHNICITY: A greater percentage of Asian women have dense breasts.
HEREDITY: Breast density can be inherited.
HRT: Density increases in women on hormone replacement therapy.
BREAST SIZE: Smaller breast size is related to higher density.
PREGNANCY/ BREASTFEEDING: Breasts become denser during this time.
WEIGHT: A higher BMI is inversely related to density.
AROMATASE INHIBITORS AND TAMOXIFEN: The use of these cancer drugs decreases density.
Studies show that regular mammograms reduce mortality. Even if you do not have dense breasts, other factors may still place you at increased risk. Density is a significant risk factor but there are many others. Talk to your doctor/nurse practitioner and discuss your risk.
Complete the IBIS risk calculator on your own or with your provider. Women considered to be at high risk will likely be sent for an MRI, as well as a mammogram. In Ontario and Nova Scotia, high risk is 25% and over life time risk. In Alberta and the US, over 20% is considered high risk. What is your lifetime risk score? Check out the IBIS risk calculator here


Why Breast Density Matters?
Dense breasts make it harder for doctors to spot cancer because both cancer and dense breast tissue appear white on mammograms. A camouflage effect is created.
Dense breasts make it harder for doctors to spot cancer because both cancer and dense tissue appear white on mammograms. A camouflage effect is created. Why is cancer easier to see in a fatty breast? Fatty tissue allows greater X-ray penetration and shows as black or dark grey on a mammogram; the contrast makes cancer easier to detect in fatty breasts. 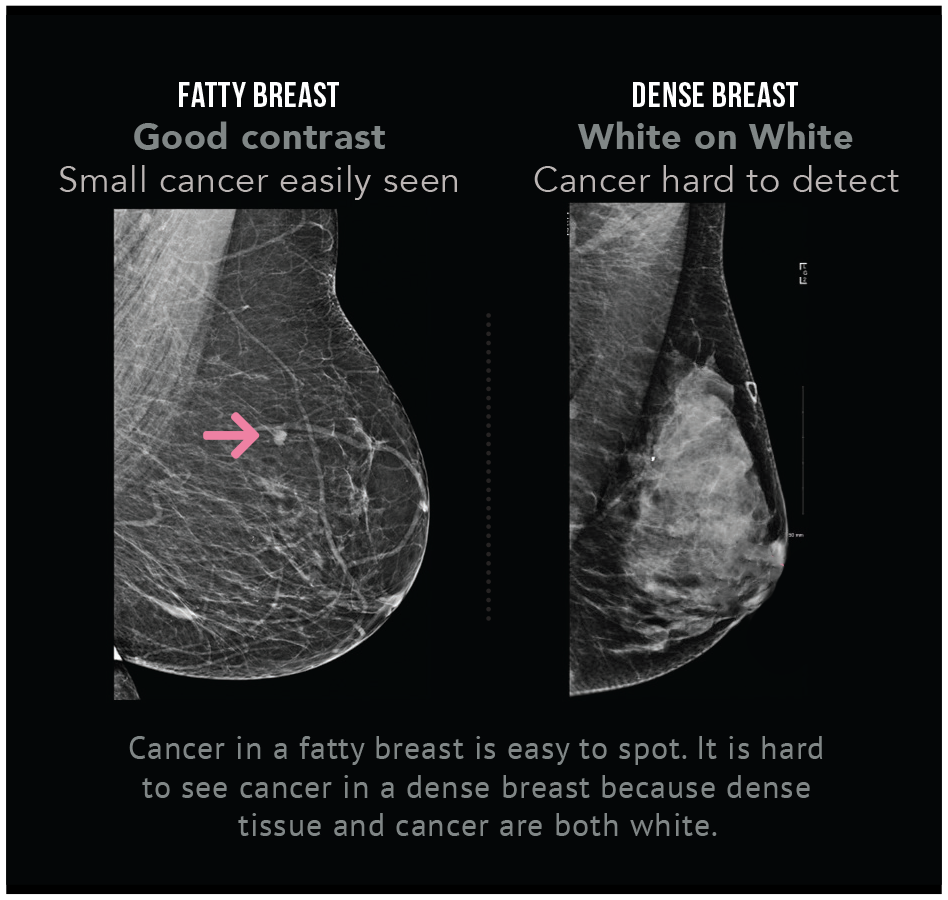
Is 3D Mammogram (TOMOSYNTHESIS) more effective for dense breasts?
Tomosynthesis (3D mammogram) is available in a few provinces as a screening tool, but for now is mostly used as a diagnostic tool. It increases the detection of invasive cancer by an additional 1-2 cancers per 1000 women. However, its effectiveness declines as the density increases. Tomosynthesis does not detect as many cancers in women with the densest breasts (Category D).
Supplementary ultrasound detects more cancers in dense breasts than Tomosynthesis. The evidence for the past 40 years shows that mammography is not enough for women with dense breasts.
The two greatest risk factors for breast cancer are being a female and getting older. Breast density is one of many other risk factors.
A recent large scale study shows breast density is a more prevalent risk factor than family history. The greater the density, the higher the risk of getting breast cancer.
Women with the highest level of density (Category D) are 4-6 times more likely to get cancer than women with the lowest (Category A).
Since mammograms miss about 40% of cancers in the densest breasts, cancer found in dense breasts is often detected at a later stage, possibly making the prognosis worse.
References:
Boyd, N., Guo, H., Martin, L., Sun, L., Stone, J., Fishel, E., Jong, R., Hislop, G., Chiarelli, A., Minkin, S., and Yaffe, M. (2007, Jan.). Mammographic density and the risk and detection of breast cancer. New England Journal of Medicine, 356:227-236. View Study
Engmann N, Golmakani M, Miglioretti D, Sprague B, Kerlikowske K, for the Breast Cancer Surveillance Consortium. (2017, Feb 2.)Population-Attributable Risk Proportion of Clinical Risk Factors for Breast Cancer. JAMA Oncol. View Study
Finding Out My Density
How can I find out my density?
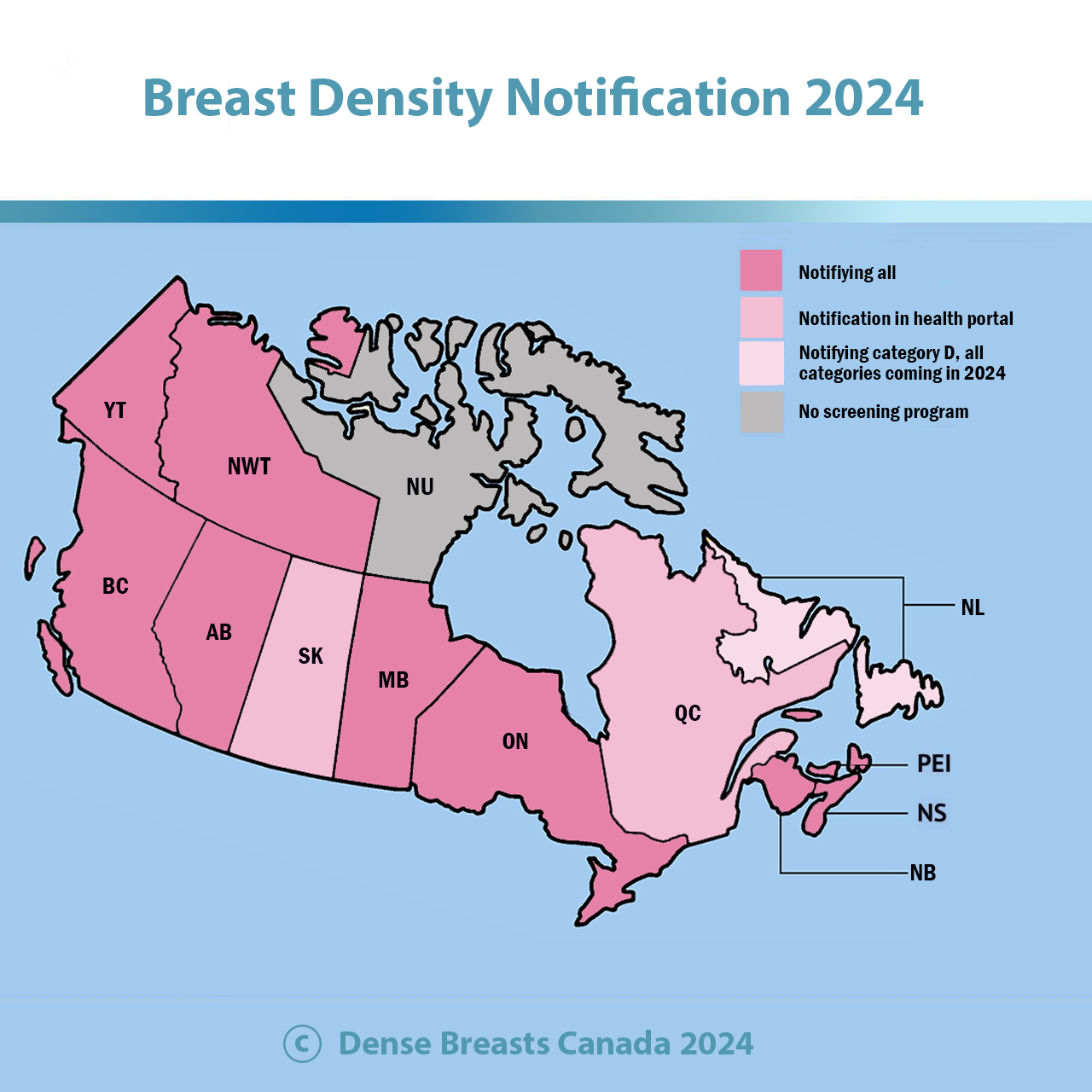
Dense Breasts Canada was successful in getting breast density notification implemented on Oct.1, 2020. Anyone having a screening mammogram will be informed of their breast density category in their mammogram results letter: A, B, C, or D. Check your letter that comes in the mail.
Category C and D are dense breasts and women in these categories can benefit from additional screening.
Your healthcare provider also receives a report that has your density category.
What should I do if I have dense breasts?
1. Please discuss optimal screening for you with your provider, based on all your risk factors. Having dense breasts increases your risk, but you may have other risk factors to consider.
2.The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 20% is considered high risk. MRI is used. When using the calculator, click the word BIRADS. Category C is called heterogeneously dense and Category D is called extremely dense. (note: Alberta is the only province that considers over 20% lifetime risk for MRI).
3. Consider additional screening: The Alberta Screening Program recommendation for healthcare providers states: For women with Category D: annual mammography and consider annual breast ultrasound and annual clinical exam. Note: Experts recommend screening ultrasound or MRI for women with both Category C and D dense breasts.
Currently, these clinics have let us know that they offer screening ultrasound to women with dense breasts, paid for by Alberta Health Services:
Mayfair, Canada Diagnostics, EFW, Pureform Radiology, Central Alberta Medical Imaging Services, Beam Radiology, Calgary Women's Imaging Clinic, Insight Medical Imaging, and MIC Medical Imaging. It is your choice where to get screened.
4. Practice self-exam and consider modification of lifestyle factors.
Advocate for change in Alberta by sending them this letter.
Breast density notification was implemented only for women with Category D density in Nov. 2018. As of December 2022, anyone can learn their breast density category in one of two ways:
1. You can ask your healthcare provider; they are now told your density category or
2. Go to your MySaskHealthRecord and see your density category on the mammogram report.
Upcoming changes: The Saskatchewan screening program is updating its system to be able to notify all individuals having a screening mammogram of their breast density in the results letter mailed to them after a screening mammogram. The update will be completed in June 2025.
Additional Screening: Individuals with Category D are asked to return annually for a mammogram.
If you have Category C or D density, you have dense breasts. Please also consider requesting supplemental screening, ie. ultrasound or MRI.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Screening at 40: Begins Jan 2025. You will be able to self-refer for a mammogram starting at age 40.
Advocate for change in Saskatchewan by sending your Health Minister this letter.
Dense Breasts Canada and patient advocates were successful in getting breast density notification implemented on Jan. 5, 2021. Anyone having a screening mammogram will be informed of their breast density category in the mammogram results letter mailed to them: A, B, C or D. Category C and D are dense breasts.
Evidence shows ultrasound or MRI are recommended for women with dense breasts as they find additional cancers that have been missed on mammogram.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Advocate for change in Manitoba by sending them this letter.
Update: Dense Breasts Canada's advocacy has been successful in Ontario. All women having a screening mammogram are directly informed of their breast density in their mammogram results letter mailed to them. This began July 21, 2023. If you had a mammogram before this date, you can find out your breast density category by asking your health care provider: is it A, B, C, or D?
Category C and D are dense breasts and women with dense breasts can benefit from additional screening.
If you do not have a healthcare provider, you can call the OBSP and they will tell you your density: 1 800 668 9304
Currently, only women with Category D are asked to return annually for a mammogram, instead of every two years. However, dense breasts refer to Category C as well. Women with Category C should consider requesting additional screening, such as ultrasound or MRI. If your healthcare provider will not provide you with a requisition for additional screening, please take a look at our conversation tips in the footer of the website. There is also a clinic in downtown Toronto that offers Automated Breast Ultrasound privately.
NEWS: In December 2023 Ontario Health announced a recommendation for additional screening for individuals with Category D. The recommendation is now being implemented. You can request a MRI every 2 years or a mammogram with ultrasound every year. You need a requisition from your healthcare provider. Read more here and you can print this off for your provider too. https://www.cancercareontario.ca/en/guidelines-advice/cancer-continuum/screening/breast-density-provider-information
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Read our press release on breast density notification:
QUEBEC: Your mammogram report sent to your healthcare provider has a description of your density in percentages. Every report has the density. You will NOT be notified directly but you can find out your density by asking. The density information is on the third line of the report. Women with over 75% density and a family history are offered screening ultrasound.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
We continue to advocate for direct notification and if you would like to express your concerns about the withholding of health information, please contact The Health Minister, The Honourable Christian Dubé
ministre@msss.gouv.qc.ca
Advocate for change in Quebec by sending them this letter.
NOVA SCOTIA: Dense Breasts Canada was successful in getting breast density notification implemented in Nova Scotia October 29, 2019. Anyone having a screening mammogram will be informed of their breast density category in their mammogram results letter: A, B, C, or D. Category C and D are dense breasts.
As of 2023, individuals with Category D density are offered annual mammograms.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Please note: Women with dense breasts can benefit from additional screening, such as ultrasound. However, GP requisitions for ultrasound are refused. This is the only province where this is happening. If you would like to help us advocate, please contact us at info@densebreastscanada.ca and please contact Premier Tim Houston premier@novascotia.ca to tell him that this situation is putting women's lives at risk. We also have a letter in the footer of our website.
July 2024 Letter to Premier Houston:
https://densebreastscanada.ca/wp-content/uploads/2024/07/Letter-to-Premier-Houston-July-22-2024-.pdf
Powerpoint Presentation to Nova Scotia MLAs on the need for additional screening. https://densebreastscanada.ca/wp-content/uploads/2024/02/Nova-Scotia-Presentation-The-need-for-additional-screening-for-women-with-dense-breasts-Feb-23-2024.pptx
Briefing Note: https://densebreastscanada.ca/wp-content/uploads/2024/03/Nova-Scotia-Breast-Cancer-Screening-Issues-2024.docx
NEW BRUNSWICK: Breast density notification for all women was implemented in New Brunswick in July 2020. You will be informed of your breast density category in your mammogram results letter: A, B, C, or D. Category C and D are dense breasts.
Please discuss optimal screening for you with your provider, based on all your risk factors. Women with dense breasts can benefit from additional screening, i.e. ultrasound or MRI. Read more on our Get Informed page.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used for this category. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
New Brunswick Breast Density Notification Press Release
PEI: Breast density notification for all women was implemented in January 2020. You will be informed of your breast density category in your mammogram results letter: A, B, C or D. Category C and D are dense breasts. Women with dense breasts can benefit from additional screening.
The government committed to screening ultrasound for women in Category D in 2018 and has not kept its commitment.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk and MRI is used. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
NEWFOUNDLAND/LABRADOR:
You are not provided with any information at this time, but change is underway. Currently, your healthcare provider is notified of your density category: A, B, C or D. Women in Category D are notified in the mail and asked to return for an annual mammogram.
A software update is under way and it is expected that all women will be informed of their breast density category in their mammogram results letter: A, B, C or D as of Fall 2024.
Please check with your GP for your breast density in the interim and discuss optimal screening for you, based on all your risk factors. Women with dense breasts can benefit from additional screening.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
How can I find out my density?
Dense Breasts Canada was successful in getting breast density notification implemented on Oct.15, 2018. Anyone having a screening mammogram will be informed of their breast density category: A, B, C, or D in their results letter. Check the letter that comes in the mail.
Category C and D are dense breasts and women in these categories can benefit from additional screening.
Your healthcare provider also receives a report that has your density category.
What should I do if I have dense breasts?
1. Please discuss the screening that best meets your needs with your provider, based on ALL your risk factors. Having dense breasts increases your risk, but you may have other risk factors to consider as well.
2.The IBIS risk calculator is recommended and can be found here When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used. When using the calculator, click the word BIRADS. Category C is called "Heterogeneously dense" and Category D is called "Extremely dense."
3. Practice self-exam as mammogram accuracy is less in dense breasts. Consider modification of lifestyle factors.
4. Consider additional screening. Experts recommend ultrasound or MRI (depends on overall risk) for women with both Category C and D dense breasts. You can request a requisition from your healthcare provider.
Currently, these locations offer screening ultrasound to women with dense breasts, paid for by MSP. A requisition is needed.
Vancouver: X-ray 505. Note screening ultrasound is only available for patients who have their mammograms there.
Victoria: West Coast Medical Imaging, Fort St. for Vancouver Island residents-using Automated Breast Ultrasound
Victoria: Victoria General Hospital for Victoria residents
Prince George: University Hospital of Northern British Columbia
Vernon: Vernon Jubilee: Category D only
Kamloops: Royal Inland Hospital: Category D. Also available for Category C patients with a lifetime risk of breast cancer calculated at >20-25%.
Nainaimo: Nanaimo Regional General Hospital: MRI for Category D
Shuswap Lake: Shuswap Lake General Hospital if mammogram is done at Vernon or Salmon Arm
Port Alberni: West Coast General Hospital.
East Kootenay: East Kootenay Regional Hospital
Chilliwack: Chilliwack General Hospital: Ultrasound for Category C and D only for patients with a 1st degree relative with breast cancer or BRCA gene
This list was last updated in September 2024. Please let us know of any additional locations.
Please sign this letter to the government asking for increased access
Breast Density Notification BC Press Release
Advocate for more access to additional screening in British Columbia in by sending them this letter.
NWT: As of March 1, 2024 All women having a screening mammogram are notified of their breast density in the mammogram results letter mailed to them. Category C and D are considered to be dense breasts. Women assessed as category D density are asked to return for annual mammograms. Women with dense breasts can benefit from supplemental screening ultrasound. This is available for women with Category D density and is an official guideline from the Dept of Health.
Yukon: As of January 1, 2024: All women having a screening mammogram are notified of their breast density in the mammogram results letter mailed to them. Category C and D are considered to be dense breasts. Women assessed as category D density are asked to return for annual mammograms. Women with dense breasts can benefit from supplemental screening ultrasound, however this is not available in the Yukon at this time.
What If I Have Dense Breasts?
Discuss your density category and any other risk factors such as genetics, family history, and previous biopsies so that your overall cancer risk is understood.
Discuss your density category and any other risk factors such as genetics, family history, previous biopsies, etc. so that your overall cancer risk is understood. Evidence shows dense breasts are a more prevalent risk factor for breast cancer than family history.
If you have dense breasts, talk to your doctor/nurse practitioner about having additional screening, such as ultrasound because a "NORMAL" mammogram result may not be accurate. Dense tissue can mask cancer. Ultrasound finds additional cancers. You are the best advocate for your health and you may need to advocate for additional testing.
HOW TO ADVOCATE FOR ADDITIONAL SCREENING
If you want added screening, advocate for yourself and let your doctor/nurse practitioner know you are aware of the following risks:
- The increased cancer risk associated with dense breasts. Dense breasts are an independent risk factor. Dense breasts are a more prevalent risk factor than family history.
- The unreliability of mammography for dense breasts because of the camouflaging effect. Both cancer and dense tissue appear white on a mammogram. This affects both categories of dense breasts.
- The high level of interval cancers for women with dense breasts- cancers detected in between screenings when a woman feels a lump after a negative mammogram.
- The proven ability of ultrasound and MRI to detect additional cancerous tumours missed by mammogram
Remember: In most cases, when extra screening is done, women are NOT found to have breast cancer.
- Speak with your doctor about your breast density, all breast cancer risk factors and your best screening options.
- Perform regular self-exams between screenings. A normal mammogram result may not be accurate.
- To improve early detection, consider additional screening, such as ultrasound (or MRI if you are considered high risk).
- Consider modifying lifestyle factors such as diet, exercise, alcohol intake and hormone use to decrease cancer risk.
- Continue to have mammograms because they can detect calcifications, which can be the earliest sign of cancer.
Ultrasound can detect a small cancer in an early stage before it spreads to lymph nodes.
In women with dense breasts, studies show that for every 1000 women screened, ultrasound finds another 2-3 cancers that were not seen on mammogram.
Several large studies have shown that supplementing mammograms with ultrasound can increase detection up to 97% in women with dense breasts.
It has been known since 1995, when the journal Cancer published the first paper, that ultrasound detects small, invasive node negative cancers in women with dense breasts.
An RCT of supplementary ultrasound screening is underway in Japan, and is showing greater cancer detection, and reduced interval cancers.
Ultrasound is used when an abnormality is detected by mammogram or clinical exam. It is not used routinely for screening because it is a sensitive test and can sometimes result in false positives – an abnormality that is not cancer. False positives are inevitable in screening and very few tests will show cancer. If you want to have an ultrasound, ask and advocate for yourself. Ultrasounds, in addition to mammography, are important for women with dense breasts because mammograms can miss cancers due to the masking effect of dense tissue.
If you have dense breasts and would like an ultrasound, but your doctor/nurse practitioner will not order it, please check out our conversation tips on what to say. To advocate effectively, we have prepared this list of potential arguments you may face. Science is on your side and decades of evidence showing the benefits of ultrasound. Here is the tip sheet. https://densebreastscanada.ca/wp-content/uploads/2022/02/Script-for-women-with-dense-breasts-who-want-a-screening-ultrasound.pdf
If you like, you can look into private facilities in your province that offer ultrasound without a doctor’s requisition.
Ontario Residents: There is a private clinic in Toronto 3D Automated Breast Ultrasound (ABUS). Private insurance may cover some of the cost. ABUS was approved by Health Canada in 2011 as a screening tool. You do not need a doctor’s/nurse practitioner’s referral. More information about private options can be found in the Screening Options Section.
BC Residents: UPDATE January 2019. Screening ultrasound for women with dense breasts is now covered by MSP if your doctor/nurse practitioner is prepared to give you an ultrasound. If not, there are imaging facilities that provide hand held ultrasound without a requisition. If you do not have a requisition, screening ultrasound is an out of pocket expense in BC (around $250).
You have dense breasts and are denied a screening ultrasound or want an ultrasound. So, you’ve had a mammogram and learned you have dense breasts. Since dense tissue can mask cancer on a mammogram, you would like additional screening. You need a requisition for a screening ultrasound, but your health care provider will not provide one or needs to be convinced. We’ve designed a script to help you advocate for yourself and overcome any potential barriers while having a conversation with your health care provider.
If your health care provider says: The Canadian breast cancer screening guidelines do not recommend screening ultrasounds for women with dense breasts.
You can respond: I understand that is the recommendation but since there is an increased cancer risk with dense breasts and since mammograms are not as effective because of the masking effect, I would like to schedule an ultrasound to be safe.
Additional information: Since 1995, ultrasound has been proven in multiple studies to detect additional cancerous tumours missed by mammogram.[1]
If your health care provider says: You don’t have a family history or any other risk factors and so you don’t need to worry about additional screening.
You can respond: Dense breasts are actually a more prevalent risk factor than family history.[2] Most women diagnosed with breast cancer have no risk factors they are aware of. I would like to go ahead and schedule an ultrasound.
**If it applies to you, you can remind your health care provider that Black, Asian and Hispanic women are at an increased risk for breast cancer at a younger age than white women.[3]
If your health care provider says: Having a screening ultrasound can result in a “false positive”, meaning you will be recalled for more testing. These tests can create anxiety for you.
You can respond: I understand that there’s a chance that more tests will be needed if something is picked up, but I’m not very worried about being recalled. I’d rather be safe than sorry. I understand any anxiety I experience will be short-lived if I have a normal result. And if the result is not normal, I’d prefer to have cancer found at an early stage, rather than a later stage. I would like to go ahead and schedule an ultrasound.
[1] https://acsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/1097-0142(19950815)76:4%3C626::AID-CNCR2820760413%3E3.0.CO;2-Z
[2] https://jamanetwork.com/journals/jamaoncology/article-abstract/2599991
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5875337/?tool=pmcentrez&report=abstract
3D ultrasound, also know as Automated Breast Ultrasound (ABUS) uses sound waves. Thousands of images are created and software reconstructs images in 3D.
Automated Breast Ultrasound (ABUS) was approved by Health Canada as a screening tool in 2011 and as an adjunct to mammography for women with no symptoms for breast cancer. Evidence shows it finds up to an additional 3.6 cancers per 1000 women screened. It is currently available privately for screening in Toronto. It is readily available in Alberta and paid for under provincial insurance.
Private insurance may cover some of the cost in Ontario. You do not need a doctor’s/nurse practitioner’s referral if you are paying privately in Ontario.
YES! Mammograms are proven to reduce breast cancer deaths. Mammograms can reliably detect suspicious calcifications. Ultrasound/ABUS do not replace mammograms; they should be used in addition to mammography.
A breast cancer risk calculator is a tool that can help you and your doctor better understand your risk and make informed decisions. We’re posting the TYRER-CUZICK 8 model because it’s just been updated to include breast density as a risk factor. It’s a well-studied and widely-used model that is easy and quick. Just click Imperial Units and if you know your density click BIRADS. If you don’t know your density, you can still use it and retry it when you find out your density. The model calculates 10 year risk and lifetime risk. Check it out.

Screening for Canadian Women with Dense Breasts
The following screening tests are described below: Mammography, Ultrasound, 3D Ultrasound (ABUS), MRI, Tomosynthesis.
Mammography reduces mortality from breast cancer, but it is an imperfect screening tool for women with dense breasts because it can miss cancerous tumors in dense breasts.
Mammograms can miss cancer about 40% of the time in the densest breasts. Therefore, women with dense breasts might want to consider additional screening with their mammogram. Ultrasound or MRI, when combined with mammography, significantly improves the rate of cancer detection in women with dense breasts.
In Canada, additional screening is not easily accessed. You may need to advocate for yourself.
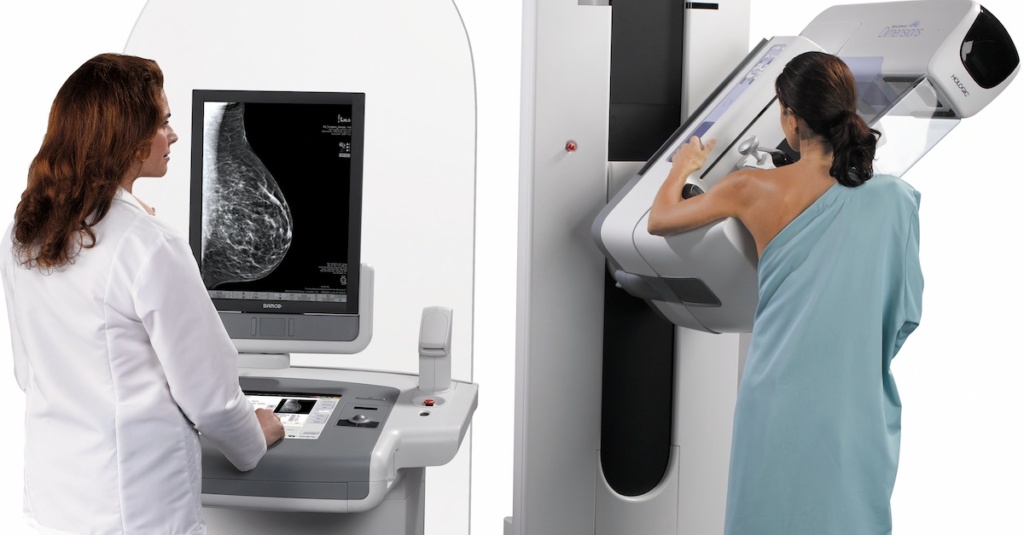
What it is: Mammography x-rays the breast from different angles. A mammogram is the only way to find out breast density.
Positives: Over the past 30 years, mammography has helped reduce deaths through early detection by more than 35%.
Limitations: For women with dense breasts, dense tissue and cancer appear white on a mammogram, making it hard for cancer to be seen. Mammography uses low-dose radiation.
Accessibility: Screening mammography is available across Canada, except Nunavut. Digital mammography is widely available and is more accurate than analog mammography in dense breasts.

What it is: Ultrasound uses high frequency sound waves to image the breast.
Positives: When used with mammography, ultrasound increases the rate of cancer detection up to 97%. It detects an additional 2-3 cancers per 1000 women. It can detect cancer in dense breasts at an early stage. It is quick, safe, and non- invasive. No radiation is involved.
Limitations: Ultrasound is a very sensitive test and is generally used for diagnostic purposes, not screening. It may identify abnormalities that require additional investigation. Ultrasound alone is not recommended as a breast cancer screening tool.
Accessibility: A requisition for ultrasound is not usually given unless there has been a suspicious finding on a mammogram, MRI or a clinical breast exam. There may be a private clinic in your city where you do not need a doctor’s/nurse practitioner’s requisition and can pay directly. UPDATE: IN BC: Screening ultrasound is now covered by MSP for women with dense breasts if the family doctor/nurse practitioner is prepared to give the woman a requisition.

What it is: This is a 3D ultrasound. Sound waves and software reconstruct breast images in a 3D plane.
Positives: ABUS can find small, invasive, node-negative cancers missed by mammography. It is radiation free.
Limitations: ABUS may identify abnormalities that are not seen on a mammogram. Some of these abnormalities may require additional ultrasound or biopsy. Remember most abnormalities are not cancerous.
Accessibility: Currently, ABUS can be found for screening purposes in Ontario, Alberta, and British Columbia.
In Ontario, there is one location in Toronto that performs screening ultrasound with ABUS. The clinic performs breast imaging and more and is called Toronto Centre for Medical Imaging. Patients wanting ABUS must pay out of pocket but some private/group insurance plans may cover part of the cost. No requisition is needed, but it is recommended to bring a CD with your latest mammograms (unless you are on Pocket Health and can email it) We are not affiliated with the clinic, so please direct any questions to them.
In Alberta, ABUS is covered under the provincial health insurance plan (AHIC) for women with dense breasts. Many clinics offer ABUS.
In British Columbia, ABUS is covered under the provincial health insurance plan for women with dense breasts (Category C and D). It is available in Victoria at West Coast Imaging. A requisition is needed. Please contact the clinic if you want more information.


What it is: Also known as 3D mammography, it creates multiple thin slices of images so that overlapping tissue is less likely to hide a cancerous tumour. The patient is positioned exactly the same way as for standard mammography.
Positives: Tomosynthesis increases the detection of invasive tumours over digital mammogram by an additional 1-2 cancers per 1000 women. When used with mammography, it decreases the false positive rate.
Limitations: Tomosynthesis does not detect as many cancers in dense breasts as ultrasound. The radiation dose may be higher than regular mammography because image acquisition takes longer. When used along with regular mammography, the radiation dose is slightly more than double.
Accessibility: Currently, Tomosynthesis is mostly being used for diagnostic purposes after an abnormality is found. However, In Alberta, patients visiting certain clinics are screened with both 2D mammography and tomosynthesis. Clinical studies are taking place in Canada to evaluate the role of tomosynthesis in screening for breast cancer.
Get the Facts. Did you know Canadian breast cancer screening guidelines are misleading, dangerous and based on flawed studies?
The 2018 breast cancer screening guidelines were made by a panel of 14 members selected by the Public Health Agency of Canada and the College of Family Physicians of Canada.
The panel did not include any experts in breast cancer screening. The panel included a psychologist, an occupational therapist and a nephrologist (kidney specialist), family doctors, nurses, a chiropractor, and an emergency room doctor. The guidelines ignored the input of experts in breast cancer diagnosis and treatment.
The Task Force stated that including breast screening experts in breast cancer diagnosis would bias the guideline development. The Task Force implied that because experts earn a living by diagnosing breast cancer, they place financial gain above the welfare of patients. We strongly disagree. In Canada, our radiologists have wait lists and their incomes do not benefit by increased demand.
The guidelines are used by Canadian family doctors and nurse practitioners. The guidelines pertain to screening for 9 million women, aged 40-74. Many provincial health agencies have adopted the guidelines in their policies. The guideline is being reviewed in 2023.
Thousands of experts think the guidelines should be rejected. The 2000 member Canadian Association of Radiologists (CAR) issued a statement rejecting the guidelines. CAR is expected to publish its own guidelines shortly.
The Canadian Society of Breast Imaging issued a statement rejecting the guidelines.
Here are just a couple of the Op-Eds written by breast cancer screening experts:
The guidelines are not based on current science. The studies used to make the guidelines are 30-50 years old and the technology used is obsolete. One of the major studies used was flawed and had compromised randomization (CNBSS). The guidelines underestimate the benefits of mammography, overstate the harms and ignore the risks of dense breasts.
Here’s why women in their 40s need mammograms:
- The incidence of breast cancer increases at age 40
- 16% of breast cancers are found in women in their 40s
- Half of fatal cancers are diagnosed by age 49
- Women who screen in the 40s are 44% less likely to die from breast cancer than women who do not have mammograms
The evidence supports women in their 40s being screened.
Based on 2 models, Dr. Martin Yaffe and Dr. Nicole Mittman estimated 400 women a year will die annually in Canada if the Task Force recommendation not to screen is followed.
A Canadian study of 2.8 million women screened for breast cancer for over 20 years showed that women 50 to 70 had a 40 % lower rate of dying from breast cancer than women who did not have mammograms. It also showed women aged 40 to 49 had a 44 % lower rate of dying from breast cancer when they participated in screening [mammography].
A recent study from Sweden showed 60% fewer deaths in the first 20 years after a cancer diagnosis, and 47% fewer deaths in the 20 years after a cancer diagnosis, in women who had mammograms, than in women who did not have mammograms.
What are the harms the Task Force asks women to consider?
A) Anxiety from a “false positive?”
The term “false positive” is misused by the task force. One might think that it means that a woman was told that she has cancer, when she does not. They use it when the mammogram shows something, and a woman is asked to return for further tests to see if cancer is present, or not. The vast majority of those women do not have cancer. Depending on the outcome of the additional imaging, sometimes a needle biopsy, done with local freezing, is performed. These are usually minimally uncomfortable.
Without doubt, being called back induces some stress, but that stress has been shown to be short-lived and is resolved when the negative results of the imaging are obtained. Usually when provided with the facts, most women are willing to put up with the stress in exchange for avoiding missing a cancer that could shorten her life or cause her to have to undergo more aggressive therapy.
B) Overdiagnosis
Overdiagnosis is the theoretical possibility that some cancers found by screening would remain harmlessly hidden in the body until the woman died of some other cause. It is likely that this occurs to some extent, but it can only be estimated. The Task Force overstates the incidence of overdiagnosis. Most experts believe that it is in the range of 1% and 10%. Overdiagnosis in more likely in older women, who may have other illnesses (heart disease) and even other cancers, that they could die of, before breast cancer might. But the probability of overdiagnosis is vanishingly small in younger women.
The decision whether to participate in screening is up to individual women with advice from their health care provider. For there to be true shared decision-making, both a woman and her physician need to have clear and accurate information on the benefits and harms of screening. Read below the misinformation Canadian experts are trying to dispel amongst women and physicians.
Addressing Misinformation about the Canadian Breast Screening Guidelines
You’re in your 40s and you’ve decided you’d like a mammogram, but in your province women in their 40s need a requisition. Your health care provider will not give you one or needs to be convinced. Or you’re in your 40s and you’ve decided you’d like a mammogram. You can self-refer in your province, but your health care provider dismisses the importance of you having a mammogram. We’ve designed a script to help you advocate for yourself and overcome any potential barriers while having a conversation with your health care provider. PLEASE NOTE IN JULY 2023, The Task Force published a newsletter where it stated that following a conversation between patient and provider, if a woman chooses to have a mammogram, she should have a mammogram. This is the clearest messaging to date from the Task Force that the decision to screen is a woman's and she should not be denied a requisition if she wants one.
If your health care provider says: The Canadian breast cancer screening guidelines do not recommend mammograms for women in their 40s.
You can respond: I understand that is the recommendation but it also states, that the decision whether or not to have a mammogram is a woman’s and that depends on the values she places on any possible benefits and harms.[1] Therefore, based on my values, this is my decision and I’ve decided to get a mammogram.
If you need a further response: You can use this quote from Task Force vice-chair Dr. Ainsley Moore, “The new guidelines are intended for an empowered position, which puts the decision-making in the hands of the individual woman in terms of what she prioritizes.”[2] Based on a woman’s values and preferences, the decision to undergo screening is conditional on the relative value a woman places on possible benefits and harms from screening. Please also refer to the July 2023 Task Force newsletter where it conveys the final decision is a woman's.
If your health care provider says: You don’t have a family history or other risk factors and so you don’t need to start screening in your 40s.
You can respond: I’m aware that the biggest risk factor for breast cancer is being a woman and that over 75% of women diagnosed with breast cancer have no risk factors.
**If it applies to you, you can remind your health care provider that Black, Asian and Hispanic women are at an increased risk for breast cancer at a younger age than white women.[3]
If your health care provider says: Having a mammogram can result in a “false positive”, meaning you may be recalled for more testing. These tests can create anxiety for you.
You can respond: I understand there’s a chance that more tests will be needed after my mammogram to make sure there is no cancer, but I’m not very worried about being recalled. I understand that less than 10% of women are recalled.[4] I’d rather be safe than sorry. I understand any anxiety I experience will be short-lived if I have a normal result. And if the result is not normal, I’d prefer to have cancer found at an early stage, rather than a later stage.
If your health care provider says: Having a mammogram can result in over-diagnosis. That means finding a cancer that if left untreated would never cause you any harm, but if detected requires treatment and surgery.
You can respond: I understand and I’m willing to accept that I may be treated for something that might never have become a problem if left untreated. Again, better safe than sorry.
If your health care provider says: This graphic shows that out of 1000 women who have a mammogram, only 1 life is saved.
Your response: I learned the Canadian Society of Breast Imaging states 2 lives are saved.[5] I also know that finding cancer early means I may avoid harsh medical treatments like chemotherapy and mastectomy that can reduce the quality of my life.
As stated in the Canadian guideline, the decision to have a mammogram is yours and therefore you have a right to have a mammogram in your 40s, no matter what province you live in.
[1] https://canadiantaskforce.ca/guidelines/published-guidelines/breast-cancer-update/
[2] https://www.ctvnews.ca/health/mammogram-guidelines-now-consider-women-s-personal-values-not-just-age-risk-1.4211240
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5875337/?tool=pmcentrez&report=abstract
[4] http://www.bccancer.bc.ca/screening/breast/results
[5]https://csbi.ca/education/
The guidelines are currently under review and it is important to show our political representatives that Canadian women need guidelines made with expert input and based on current evidence.
Write your MP
Write Health Minister Mark Holland and Associate Health Minister Ya'ara Saks.
Watch Health Critic Don Davies question the Health Minister
The Health Minister on the government's new breast cancer screening guidelines
The Liberals on Canada's new breast cancer screening guidelines